Vitamin D deficiency is very common worldwide. Reduced intake of vitamin D rich food items and sun exposure are the primary factors leading to vitamin D deficiency.
Vitamin D deficiency causes hypocalcemia and hypophosphatemia leading to reduced mineralization of bones.
Other than its effects on bones, it is now thought to have effects on almost every organ of the body and has some protective role in cardiovascular diseases, diabetes, and some cancers.
Calcium homeostasis requires vitamin D

Calcium is an important micronutrient that is very essential for bone health. Calcium in the body is regulated by parathyroid hormone, calcitonin, and Vitamin D or cholecalciferol.
Vitamin D and calcium deficiency can lead to increased fragility of bones. Decreased mineralization of bone is called osteopenia and decreased matrix or the protein part is called osteoporosis.
For healthy bones, one needs to have a good bony matrix which makes the core part of the bone as well as enough calcium in the bones to mineralize the bone.
Vitamin-D deficiency results in bone fractures
People who have weak bones are at risk of fractures. Important sites of fracture in the body are hip bones, spine, long bones and wrist bones.
Patients with decreased mineralization of the bones or osteopenia can present with bony pains and weakness of the thighs arms and shoulders muscles.
This is manifested by the inability to get up from squatting position, climb up stairs or comb hair. Patients with decrease matrix or osteoporosis may maybe asymptomatic until they have fractures or may note a reduction in their height.
Role of vitamin D in the prevention of bone fractures
The most important aspect in the treatment and prevention of weak bones is to take an adequate amount of calcium and Vitamin D in the diet and exercise regularly.
Foods and drinks that contain an adequate amount of calcium and Vitamin D include dairy products like milk, yogurt, cheese, ice cream, green vegetables like kale, collard green, and broccoli, nuts, cooked salmon, fish, and cod liver oil are also rich in calcium and Vitamin D.
Sunlight is an important factor in the synthesis of Vitamin D.
Medications which are used as supplements include cholecalciferol and Calcium.
Cholecalciferol has flooded the markets in the form of tablets, capsules, and injectable in different doses and formulations. Adequate calcium intake is important for vitamin D to function properly.
What is vitamin-D deficiency and, insufficiency?
Subclinical vitamin D deficiency or insufficiency is common and is defined is levels lower than the normal Vitamin D levels without clinical signs.
A normal level of cholecalciferol is defined is 25 hydroxy-vitamin D of more than 30 ng/ml.
Vitamin D insufficiency is defined as levels between 20 and 30 ng/ml and vitamin D deficiency is defined as vitamin D levels of less than 20 ng/ml.
Patients who are prescribed cholecalciferol and Calcium should have a repeat blood test 3 months after the beginning of treatment.
Daily requirements of vitamin D
The maximum daily intake of vitamin D is not clear but the tolerable upper level has been defined as 100 mcg or 4000 IU daily for healthy adults and children.
The recommended dietary allowance of Vitamin D is 600 IU or 15 mcg for people aged less than 70 years and 800 IU or 20 mcg for patients more than 70 years of age.
Causes of calcium and vitamin D deficiency:
Patients who have less than optimal intake of calcium and Vitamin D in their diet can have hypocalcemia and vitamin-D deficiency.
This is especially found in patients in developing countries where people have inadequate calcium and vitamin-D in their diets. Children, pregnant and lactating women and elderly people in developing countries are at special risk.

Individuals who have problems in their gastrointestinal tract like those with a chronic diarrheal state, malabsorption like celiac disease, patients who have chronic pancreatitis and patients with liver diseases.
Patients with cholestatic liver diseases and chronic pancreatitis can develop a deficiency of fat-soluble vitamins including vitamin-D.
Those patients who have liver or renal problems can also present with Vitamin-D and Calcium deficiency because of the inability to activate cholecalciferol in the body.
Patients who have subnormal secretion of parathyroid hormone-like those with hypoparathyroidism or patients who have undergone thyroid surgery may have incidental removal of their parathyroid glands and can present with hypocalcemia and vitamin-D deficiency.
Other disorders of hypocalcemia and vitamin-D deficiency include steroid intake and rare disorders like vitamin D resistant rickets
Adverse effects of calcium and Vitamin D, when in excess
People who are using Vitamin D and Calcium supplements in excess can develop the following adverse effects
Constipation and stomach problems
Hypercalcemia or increased calcium can cause stomach ulcers and decrease bowel movements leading to constipation.
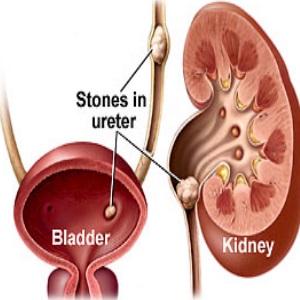
Kidney stones
Excessive calcium intake can lead to the formation of kidney stones which may present with severe abdominal pain and recurrent urinary tract infections.
Neuropsychiatric symptoms:
Patients with hypercalcemia may develop irritability, become drowsy or present with psychosis. Severe hypercalcemia also called the hypercalcemic crisis can be life-threatening in certain patients.
Patients may develop polyuria and be markedly dehydrated. Dehydration itself can cause elevation of blood calcium levels.
Increased calcium in the body without excessive calcium or Vitamin-D intake:
There are certain conditions where patients can have hypercalcemia without a history of vitamin D or calcium supplementation.
Hyperparathyroidism
This is a disease of parathyroid gland situated in front of the neck in close proximity to the thyroid gland. The parathyroid glands are producing an excess of parathyroid hormone which in turn mobilize calcium from the bones.
This leads to hypercalcemia but the bones can become weak. The major cause of increased parathyroid hormone secretion is secondary hyperparathyroidism in patients with renal failure.

Patients with secondary hyperparathyroidism have hypocalcemia which stimulates the parathyroid gland to secrete excess parathyroid hormone. Other causes of hyperparathyroidism include parathyroid hyperplasia and adenoma.
Patients with these conditions can have hypercalcemia and increased parathyroid hormone.
Multiple Myeloma.

This is a disorder of bone marrow producing an excess of clonal plasma cells. Patients with multiple myeloma can present with renal failure, anemia, skeletal pains, repeated infections, and hypercalcemia.
Sarcoidosis and other granulomatous disorders.
Macrophages and epithelioid cells in these conditions can produce excess Vitamin-D leading to hypercalcemia.
Miscellaneous
Drugs like thiazide diuretics and cancers invading the bones scan present with hypercalcemia. Sometimes cancers do not invade the bones but produce parathyroid hormone-related peptide (PTH-rP) causing hypercalcemia.
Role of vitamin D in extraskeletal health:
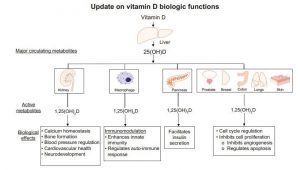
In addition to skeletal health, vitamin-D plays an important role in many other cellular functions.
Muscle weakness:
A lot of studies have shown a positive correlation between muscle function and vitamin-D levels. Vitamin d supplementation has been shown to improve balance, muscle strength, physical performance and gait in elderly patients.
Cancers
The association of vitamin-D deficiency with cancers came from the idea that people at high altitude are at higher risk of cancers. Later ultraviolet B exposure at high altitude was linked with vitamin-D status.
Extensive studies have shown that active form of vitamin-D or its metabolites can decrease cell proliferation which is the primary defect in cancers.
The World Health Organization (WHO) working group identified colon cancer as the greatest risk associated with poor vitamin-D status. Other studies have found an increased risk of pancreatic cancers in patients with higher levels of vitamin D.
Immune system:

Since vitamin d is an inhibitor of dendritic cells maturation, theoretically its deficiency can increase the risk of autoimmune diseases.
In humans, vitamin d deficiency has been associated with type 1 diabetes mellitus, multiple sclerosis, and inflammatory bowel diseases. Patients with vitamin d deficiency have been shown to be at risk of infections.
vitamin d deficiency has been inversely correlated with hypertension and body mass index. Patients with vitamin D levels of less than 20 ng/ml were found to have increased risk of angina, myocardial infarction, heart failure, and peripheral arterial diseases.

Vitamin d deficiency has been associated with an increased risk of diabetes and metabolic syndrome. Vitamin d supplementation has been shown to increase insulin sensitivity in type 2 diabetes mellitus.
Neuropsychiatric functions:
vitamin d deficiency has been associated with depression, Alzheimer’s and schizophrenia.
Book your appointment if you have calcium or vitamin D deficiency