Diabetic patients need to know their target blood sugars. When the target blood sugars are known, modifications in diet, exercise routine and changes in medications become easy.
Normalization of plasma glucose is difficult and maintaining a euglycemic state for a longer period of time is extremely difficult. Regardless of the level of hyperglycemia, improvement in the glycemic control decreases the risks of long-term complications related to hyperglycemia.
Target Blood Sugars – Role of glycated hemoglobin

Long-term glycemic control as reflected by the A1C levels should be individualized considering the patient’s age, comorbidities and presence and severity of complications of diabetes, lifestyle, occupation and the level of support from the family.
Factors to consider prior to setting the Target Blood Sugars

Target blood sugars in diabetic patients vary. This is dependent on various factors:
- Age of the patient
- Duration of diabetes
- Type of diabetes
- Treatment of diabetes
- Comorbid illnesses and
- Current status
Target Blood Sugars according to the ADA recommendations

As a general rule, the ADA (American Diabetes Association) recommends
- The fasting blood sugars between 70 mg/dl and 130 mg/dl
- 2 hours post-prandial blood sugars between 100 mg/dl and 180 mg/dl
- Glycated hemoglobin of less than 7%.
Target Blood Sugars for newly diagnosed Diabetic individuals
This generalization does not fit all patients. For example target blood sugars for a young newly diagnosed diabetic patient should be:
- Fasting blood sugars between 70 mg/dl and 115 or 120 mg/dl
- 2 hours post-meal blood sugars between 100 to 150 or 160 mg/dl and
- Glycated hemoglobin of less than 6.5%
Target Blood Sugars for DIabetic Individuals with comorbid conditions
Similarly, Target blood sugars of patients with comorbid chronic conditions may be a little high. Target blood sugars in these patients include:
- Fasting blood sugars between 90 mg/dl to 140 mg/dl and sometimes even 150 mg/dl
- 2 hours post-prandial blood sugars between 100 mg/dl to 200 mg/dl
- Glycated hemoglobin between 7% and 7.5%.
Target Blood Sugars for pregnant patients
- Fasting Blood sugars should be less than 95 mg/dl (preferably 92 mg/dl)
- Two hours post meals blood sugars should be less than 120 mg/dl
- Glycated hemoglobin is not recommended in gestational diabetes.
Target Glycated Hemoglobin
Target HbA1C should be 7% for most patients as the ADA (American diabetes association) recommends. Elderly patients, those experiencing frequent hypoglycemia, those with complications of diabetes and have cardiovascular risk factors may have a target A1C higher than 7% (7% to 7.5%). Younger patients or newly diagnosed diabetic patients without complications, on the other hand, may have a target A1C of less than 7 % ( < 6.5%). A1C of less than 6% is not beneficial and may be harmful especially in patients with cardiovascular disease.
Goals of therapy for Diabetic individuals

Goals of the therapy in both Type 1 and Type 2 DM are to
- Eliminate hyperglycemic symptoms
- Reduce/ eliminate long-term microvascular and macrovascular complications and
- Allow the patient to live as normal life as possible.
A target level of glycemic control should be set for the patient. Furthermore, the patient should be educated regarding self-monitoring of blood glucose ( SMBG) at home and how to manage very high and especially, very low blood sugars.
Involve the whole team

Care of the diabetic patient involves a multidisciplinary team ( including a primary care provider, endocrinologist/ diabetologist, a diabetic educator and a nutritionist) and above all the individual’s input and participation. When chronic complications develop, subspecialists must be involved. Apart from the physical aspects of diabetes care, social, family, financial, cultural employment-related issues strongly impact diabetes care.
Education about DM, nutrition, and exercise:
Educating diabetic individuals about their disease, their target blood sugars, exercise, drugs, and complications allows them to assume a greater responsibility. Patients education is a continuous process with regular visits and reinforcement and has been shown to improve glycemic control. Individuals should be educated about self-monitoring of blood glucose, urine ketone monitoring (T1DM), insulin administration, diabetes management during illnesses, prevention and management of hypoglycemia, foot and skin care, nutrition, and exercise.

Primary, secondary and tertiary prevention
Primary nutritional therapy is aimed at delaying the onset of T2 DM in high-risk individuals. Secondary prevention is to delay diabetes-related complications by improving glycemic control. Tertiary prevention is directed at managing chronic complications of DM. Foods with low glycemic indices improve glycemic control.
Medical nutrition therapy

Caloric intake should match with the appropriate amount of insulin. Weight gain should be minimized. This is often seen with intensive diabetes management. In type 2 DM medical nutrition therapy (MNT) should focus on weight loss and addressing cardiovascular risk factors like hypertension and dyslipidemia.
Exercise is important for good health
Exercise recommendations for diabetic individuals

ADA recommends 150 min/week (distributed over at least 3 days) of moderate aerobic physical activity. During exercise, diabetic individuals especially type 1diabetic patients have an unpredictable glycemic response. Exercise-related hypo- or hyperglycemia can be avoided by monitoring pre-exercise plasma glucose, reducing insulin dose if plasma glucose is less than 100 mg/dl, delaying exercise if plasma glucose is more than 250 mg/dl, monitor glucose during exercise and ingest carbohydrates to prevent hypoglycemia.
Screening for diabetic complications
Individuals should be screened for cardiovascular disease with formal exercise tolerance testing if they are greater than 35 years of age, duration of diabetes is greater than 15 years for type 1 and 10 years for type 2 DM, have developed microvascular complications, Peripheral arterial disease, other risk factors of cardiovascular diseases, or autonomic neuropathy. Untreated retinopathy is a relative contraindication to vigorous exercise.

How frequent to monitor blood sugars
Monitoring of plasma glucose is very important. This includes self-monitoring of blood glucose (SMBG) and long-term glycemic status (HbA1C), a measurement of glycemic control over 2 to 3 months. The frequency of SMBG measurement should be individualized to address the goals of diabetic care.
Patients on two or three doses of insulin should frequently assess their glucose levels preferably before each meal. Patients on diet control or oral antidiabetic treatment usually require less frequent monitoring (two to four times a week). Glycated hemoglobin is the standard investigation for assessing long-term glycemic control and has strongly been associated with long-term diabetic complications.
Variations in glycated hemoglobin
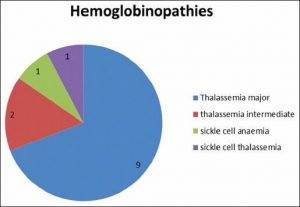
Laboratory variations, hemoglobinopathies, anemias, reticulocytosis, transfusions, and uremia may interfere with the A1C result. Patients should have A1C measured every three months if glycemic control is inadequate or therapy is changed and at least twice per year in patients achieving a glycemic goal. Glycation of other proteins, such as albumin, can be used as an alternative indicator of glycemic control especially when A1C is inaccurate like in states of anemias. Glycated albumin reflects glycemic status over the prior 2 weeks
Read More …
Complications of Diabetes Mellitus
How to diagnose Diabetes Mellitus
Brittle Diabetes – A young man living as a child