Stress-induced cardiomyopathy or Takotsubo cardiomyopathy also called apical ballooning syndrome and broken heart syndrome is increasingly being reported in the literature.
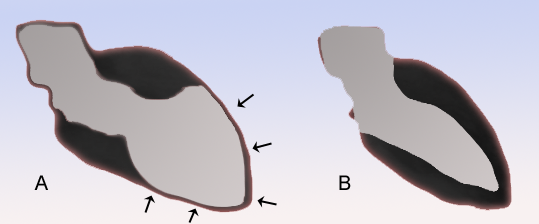
This condition sometimes mimics myocardial infarction but angiography is characteristically normal. There is apical and sometimes septal ballooning and transient systolic dysfunction.
Takotsubo cardiomyopathy – The word TAKOTSUBO
Takotsubo is a Japanese word meaning an octopus trap. The condition was named takotsubo or octopus trap because of the similarity in shapes of the apical ballooning to the octopus trap.
Broken heart syndrome or stress-induced cardiomyopathy is more common in women than men. Postmenopausal Women account for up to 80% of the cases.
Triggers of Broken Heart syndrome – Stress?
The onset of stress-induced cardiomyopathy is frequently but not always triggered by an acute medical illness or by intense emotional or physical stress (eg, the death of relatives, particularly if unexpected, domestic abuse, arguments, catastrophic medical diagnoses, devastating financial losses, and natural disasters).
Postulated mechanisms include catecholamine excess, coronary artery spasm, and microvascular dysfunction.

How stress causes stress-induced cardiomyopathy?
Physical or emotional stress causes a surge of catecholamines in the body. These hormones are responsible for the vascular tone and increasing the heart rate and contractility. With their excessive release, vessels especially coronary vessels may go into spasm leading to angina-like symptoms.
What are the symptoms of stress-induced cardiomyopathy?
Patients with stress-induced cardiomyopathy or broken heart syndrome may present like patients with angina or myocardial infarction.
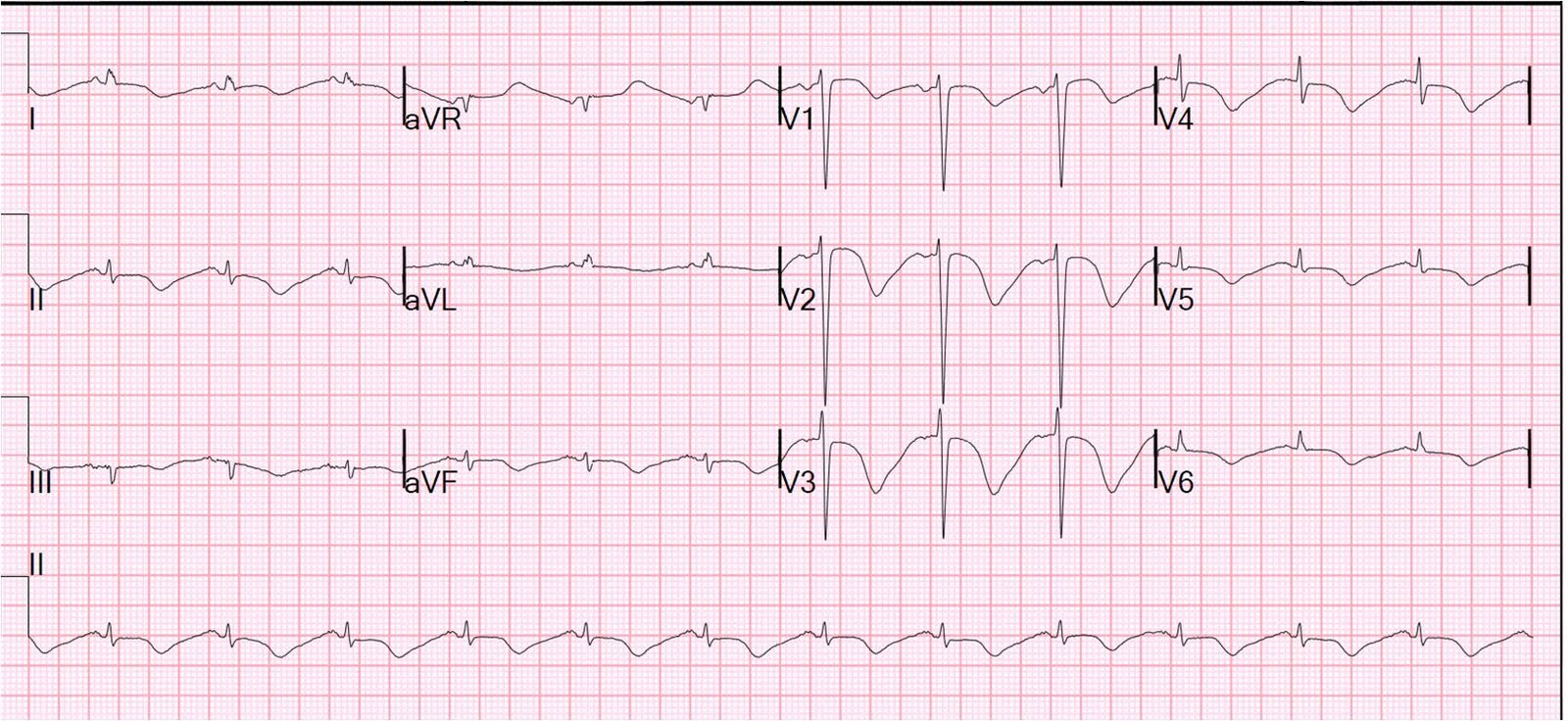
These symptoms include dyspnea, syncope, and shock. ECG may also show findings similar to myocardial infarction. However, ECG may be normal in some patients.
Acute complications of stress-induced cardiomyopathy can include heart failure, tachyarrhythmias, bradyarrhythmias, mitral regurgitation, and cardiogenic shock.
Unlike patients with myocardial infarction, cardiac biomarkers like troponins are only mildly elevated. Echocardiography usually shows apical ballooning and systolic dysfunction.
Diagnosis requires a high index of suspicion
A high index of suspicion is required to diagnose takotsubo cardiomyopathy. The diagnosis of stress-induced cardiomyopathy should be suspected in postmenopausal women who present with an acute coronary syndrome after intense psychologic stress.
Furthermore, the clinical manifestations and ECG abnormalities are out of proportion to the degree of elevation in cardiac biomarkers in these patients.
Apical ballooning (typical variant) and/or midventricular hypokinesis is usually seen on left ventriculography or echocardiography. Atypical features may be seen in a minority of patients.
These include transient left ventricular hypokinesis restricted to the midventricular segments. This is called the atypical variant or apical sparing variant without the involvement of the apex.
Coronary angiography is characteristically normal however coexistent obstructive coronaries may be seen occasionally.
A number of other syndromes in addition to stress-induced cardiomyopathy have been associated with ST-segment changes in the absence of significant coronary artery disease, including cardiac syndrome X, variant (Prinzmetal’s) angina, myocarditis, and cocaine abuse.

For diagnosis, all four of the following proposed Mayo Clinic diagnostic criteria should be met.
- Transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments with or without apical involvement. The regional wall motion abnormalities typically extend beyond a single epicardial coronary distribution. A stressful trigger is often, but not always present.
- The absence of obstructive coronary disease or angiographic evidence of acute plaque rupture.
- New electrocardiographic abnormalities (either ST-segment elevation and/or T wave inversion) or modest elevation in cardiac troponin.
- The absence of pheochromocytoma or myocarditis.
How to proceed if the patient presents in the emergency with Chest pain after an intensely stressful situation?
Just like patients with acute myocardial infarction, these patients when present to the emergency should undergo cardiac catheterization/ primary PCI (percutaneous intervention) as the usual cases of MI.
Normal coronaries and apical ballooning will point to the diagnosis, otherwise, patients can undergo PCI.
Where primary PCI is not available, patients may be treated with fibrinolytic therapy. Since Myocardial infarction is much more common, a critical coronary lesion should never be left untreated.
A Critical Coronary Lesion should never be left untreated
If PCI later shows normal coronaries and systolic function improves, the diagnosis can be either way – stress-induced cardiomyopathy or successful fibrinolysis.
- Similarly, patients with chest pain and ST segment depression or T waves inversion with elevated cardiac markers may be treated as Non-ST elevation Myocardial infarction. PCI may later suggest the correct diagnosis.
- Stress-induced cardiomyopathy may also be suggested by the Echocardiographic findings. In obstructive coronaries, hypokinetic walls correlate with the obstructive coronaries supplying that area. Contrary to that, stress-induced cardiomyopathy involves the area of hypokinesia corresponding to more than one coronary arterial supply.
Treatment of Broken heart syndrome:
Stress-induced cardiomyopathy is usually managed conservatively. Relieving the catecholamine surges via resolving the stressful situation may result in a rapid resolution of the symptoms.
Treatment of stress-induced cardiomyopathy includes ACE inhibitors, beta blockers, and diuretics as necessary for volume overload. Recovery of systolic function may take four weeks or more. However, since recurrence is common, it is better to continue with alpha/beta blockers.
Similarly, there is a high risk of left ventricular thrombus formation, anticoagulation should be given to all patients for three months or at least until severe systolic dysfunction resolves, whichever is shorter.
Mortality ranges from 0 to 8%. However, further studies are required to correctly identify the factors associated with mortality.

