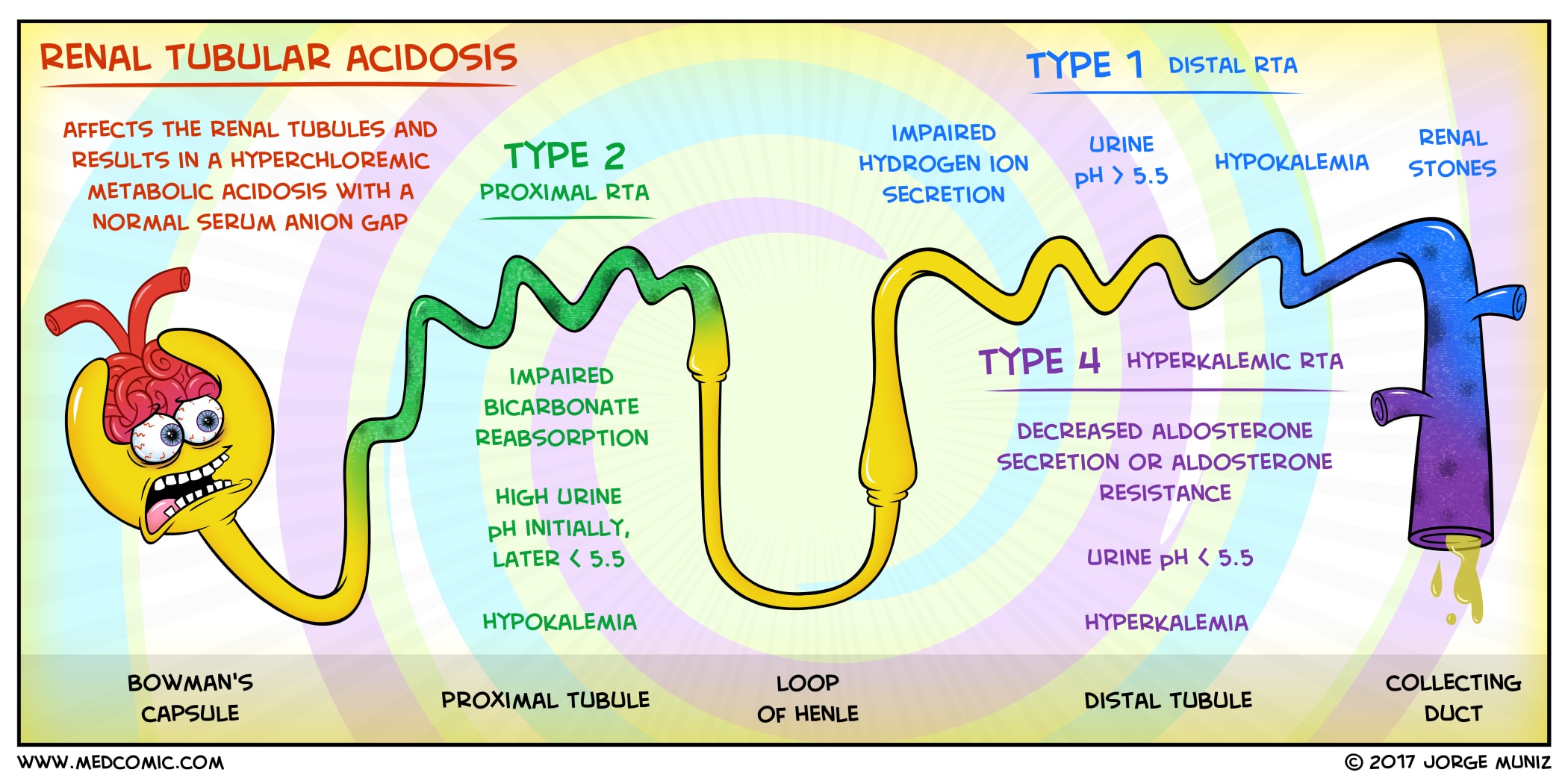
Renal tubular acidosis is a disorder of the renal tubules characterized by metabolic acidosis with a preserved renal function.
Similarly, the hormonal and other metabolic effects of the kidneys on the distant organs are also not affected.
We will briefly discuss the main types of Renal Tubular Acidosis, their clinical presentation and the differences between the various types of RTA.
Briefly about the acid-base homeostasis in the body
The normal body PH is maintained at 7.40 by the various physiological processes. The major organs responsible for maintaining body PH are the Kidneys and the lungs. Acidosis occurs either because of Hydrogen ions retention or the loss of bicarbonate from the body.
Respiratory Acidosis?
When carbon dioxide is not properly removed from the body, Respiratory acidosis occurs. This is manifested by a blood PH of less than 7.40 and partial pressure of carbon dioxide greater than 40 mmHg.
Metabolic Acidosis?
Similarly, when the PH drops to less than 7.40 and the bicarbonate levels also decrease to less than 24 mEq/l, this is metabolic acidosis. Metabolic acidosis can be classified further into two – Metabolic acidosis with a normal anion gap or a high anion gap.
The Anion gap is the difference between unmeasured anions and unmeasured cations in the body. The normal anion gap is 8 to 12 and can be calculated via the formula:
Anion gap = S. Na – (S. Cl + S. HCO3) or S.Na – S.Cl – S. HCO3
Causes of raised anion gap metabolic acidosis (Remember MUDPILES)

- Methanol intoxication
- Uremia
- Diabetic ketoacidosis, alcoholic ketoacidosis, starvation ketoacidosis
- Paraldehyde toxicity
- Isoniazid
- Lactic acidosis
- Type A: tissue ischemia
- Type B: Altered cellular metabolism
- Ethanol or ethylene glycol intoxication
- Salicylate intoxication
Causes of a normal anion gap metabolic acidosis include (remember USED CAR)

- Ureterosigmoidostomy
- Saline administration (in the face of renal dysfunction)
- Endocrine (Addisons, spironolactone, triamterene, amiloride, primary hyperparathyroidism)
- Diarrhea
- Carbonic anhydrase inhibitors
- Ammonium chloride
- Renal tubular acidosis
Renal Tubular Acidosis characterized by a normal anion gap metabolic acidosis:
Coming to RTA or renal tubular acidosis, it is always suspected when there is metabolic acidosis (Low PH and low bicarbonate) and a normal anion gap (Na- cl-bicarbonate).
RTA is a condition in which the GFR is relatively well preserved but because of the defective tubular function, metabolic acidosis develops.
Types of Renal Tubular Acidosis:
- Distal RTA or type 1 RTA (defect in renal hydrogen ion excretion)
- Proximal RTA or type 2 RTA (defect in bicarbonate reabsorption)
- Hypoaldosteronism or type 4 RTA (hypoaldosteronism)
(Type 3 RTA is sometimes labeled when there are features of both type 1 and type 2).
Distal Renal Tubular Acidosis or Type 1 RTA:
Distal RTA is characterized by a defective H+ excretion. This results in an abnormally high urine PH or alkaline urine despite systemic acidosis.
Causes of distal Renal Tubular Acidosis:
Primary:
- Idiopathic
- Familial (autosomal dominant or recessive)
Secondary:
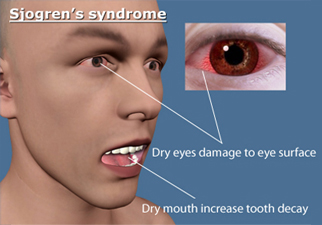
- Autoimmune disorders
- Sjögren’s syndrome
- Autoimmune hepatitis/Primary biliary cirrhosis
- Systemic lupus erythematosus
- Rheumatoid arthritis
Drugs:
- Ifosfamide
- Amphotericin B
- Lithium carbonate
- Toluene inhalation
Hypercalciuric conditions:
- Hyperparathyroidism
- Vitamin D intoxication
- Sarcoidosis
- Idiopathic hypercalciuria
Other:
- Medullary sponge kidney
- Obstructive uropathy (maybe hyperkalemic)
- Renal transplant rejection
- Wilson’s disease
- Autoimmune disorders
Distal Renal tubular acidosis present with a normal anion gap metabolic acidosis and an inappropriately high urine PH (> 5.3).
Patients usually have hypercalciuria as a result of the acidic PH on bones. Both hypercalciuria and hypocitraturia contribute to the development of nephrolithiasis and nephrocalcinosis.

Hypokalemia is frequently seen in patients with proximal and distal RTA. At times it might be so severe that patients present with paralysis and rarely respiratory muscle paralysis.
Correction of the acidosis with alkali therapy improves both calcium and potassium balance and prevent stones and nephrocalcinosis.
In contrast to the proximal RTA where a high alkali is required, in distal RTA, alkali therapy is only modestly required
Briefly about proximal Renal Tubular Acidosis:
Proximal RTA may present with an isolated tubular defect or as Fanconi syndrome (generalized tubular dysfunction. Bicarbonate is not reabsorbed and lost in the urine.
In a generalized disorder, bicarbonaturia may be accompanied by glucosuria, aminoaciduria, phosphaturia, uricosuria, and tubular proteinuria.
Causes of proximal RTA
Primary:
- Idiopathic (sporadic)
- Familial
- Recessive – proximal tubule cell sodium bicarbonate cotransporter (NBCe1) defect
- Recessive – carbonic anhydrase type 2 deficiency
- Cystinosis
- Tyrosinemia
- Hereditary fructose intolerance
- Galactosemia
- Glycogen storage disease (type I)
- Wilson’s disease
- Lowe’s syndrome
Acquired disorders:
- Drugs
- Ifosfamide
- Tenofovir
- Carbonic anhydrase inhibitors – acetazolamide; topiramate
- Aminoglycosides
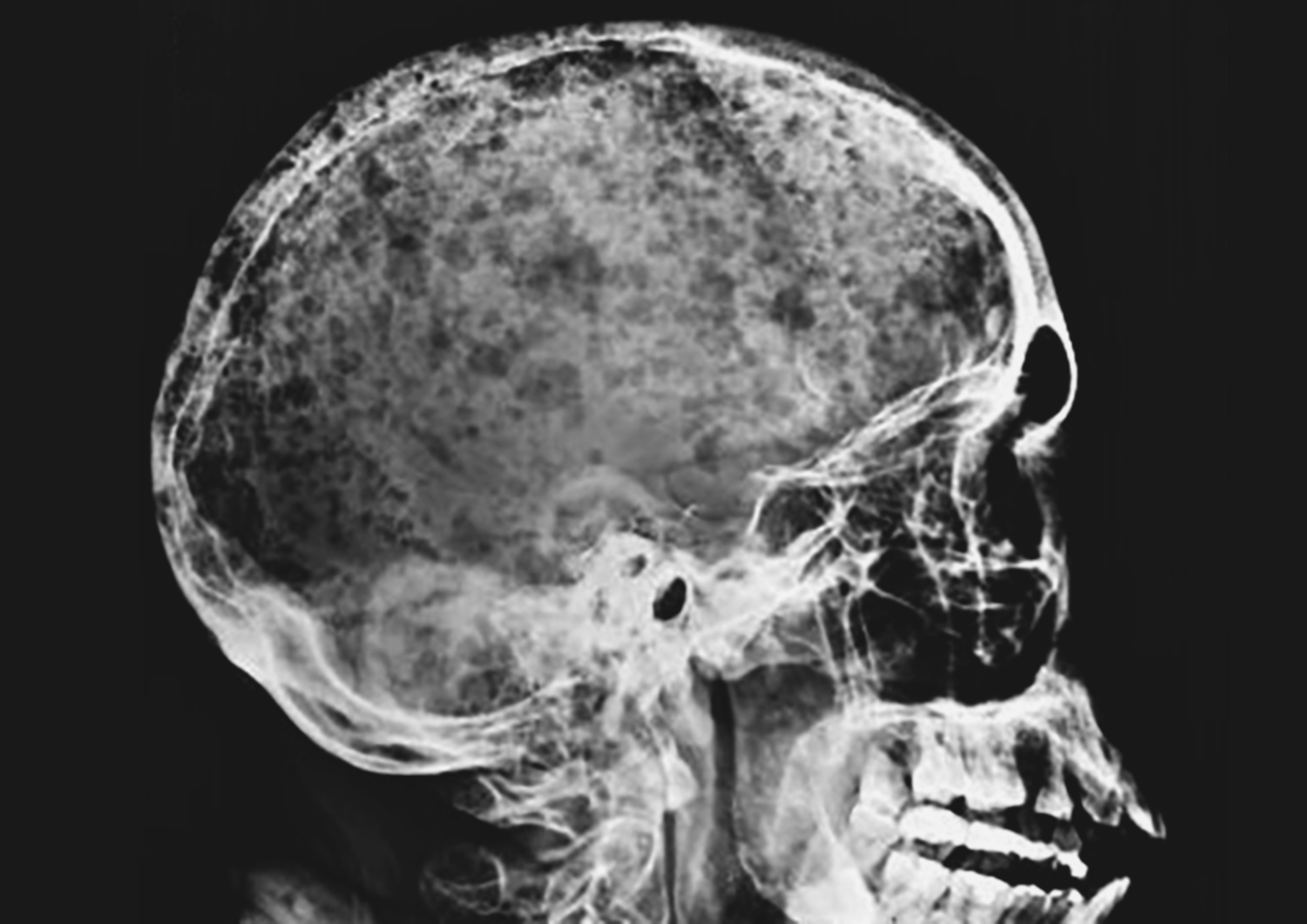
- M-Protein disorders
- Amyloidosis
- Multiple myeloma/ light chain disease
- Heavy metals
- Lead
- Cadmium
- Mercury
- Copper
- Vitamin D deficiency
- Renal transplantation
- Paroxysmal nocturnal hemoglobinuria
- Drugs
Almost all adult patients with Acquired Proximal Renal Tubular Acidosis require a workup for Monoclonal Gammopathy.
In patients with proximal RTA, urinary PH may vary. When the plasma bicarbonate is 16 mEq/l or greater, bicarbonate will be excreted in the urine and the PH will rise. In patients with plasma bicarbonate less than 16, the urine may be acidic (5.3 or less).
Treatment is with bicarbonate therapy, usually in very high doses.

Type 4 Renal Tubular Acidosis or Hyporeninemic Hypoaldosteronism:
Type 4 RTA is manifested by hyporeninemic hypoaldosteronism. It occurs in patients with CKD and especially diabetic nephropathy and is manifested by normal anion gap metabolic acidosis and hyperkalemia.
| Type | Type 1 | Type 2 | Type 4 |
|---|---|---|---|
| Location | Collecting Tubules, distal tubules | Proximal tubules | Adrenal |
| Acidemia | Yes (very severe) | Yes | Mild when present |
| Potassium | Hypokalemia | Hypokalemia | Hyperkalemia |
| Pathophysiology | Failure of α intercalated cells to secrete H+ and reclaim K+ | Failure of proximal tubular cells to reabsorb HCO3− | Deficiency of aldosterone, or a resistance to its effects, (hypoaldosteronism or |
Read More …
Wilson’s Disease – a case presentation and discussion
Bleeding disorder – a rare case scenario
A case scenario of Atrial Myxoma
A real case scenario of acute intermittent porphyria
A very interesting case of a young hypertensive patient
Renal Tubular Acidosis – A young female with lower limbs weakness