Hyperkalemia treatment requires stabilizing the patient, shifting potassium into the cells, removing excess potassium from the body, and finding & treating the underlying cause.
What is the normal potassium level in the plasma?
Normal Potassium in the body is 98% intracellular (inside the cells) and 2% extracellular (in the plasma)
The normal Potassium level in the plasma is between 3.5 and 5.5 mEq/L.
Na/K ATPase pump maintains this high intracellular concentration by pumping potassium in the cell in exchange for sodium ions.
The major route of excess potassium excretion is via the kidneys.
What are the Stages of Hyperkalemia?
Hyperkalemia is a serum potassium concentration greater than its normal value i.e. exceeding 5.5mEq/L.
It can be classified into
- Mild hyperkalemia: Serum potassium between 5.5 and 6.5 mEq/l
- Moderate hyperkalemia: Serum potassium between 6.5 and 8.0 mEq//l
- Severe hyperkalemia: Serum potassium of more than 8.0 mEq/L
What are the Causes of hyperkalemia?
Before initiating the work-up of hyperkalemia, the treating doctor must rule out the possibility of a lab error and pseudohyperkalemia.
Causes of pseudohyperkalemia include:
- Venipuncture technique: Venipuncture technique in which the patient is asked to clench his fist causes cell lysis releasing intracellular potassium giving a false laboratory result of hyperkalemia.
- Thrombocytosis: Thrombocytosis is an excess of platelets in the body. Hyperkalemia occurs as clotting occurs
- Leukocytosis: Leukocytosis is an excess of white blood cells in the body as in leukemia or blood cancer. Excessive cell lysis, especially the immature cells, causes the release of potassium into the plasma causing hyperkalemia.
- Acidosis: Excessive extracellular H+ ions cause activation of Na/H pump which pumps H+ ions in the cell but causes an increase in extracellular sodium. This, in turn, stimulates Na/K pump which pumps excess Na in the cell but at the cost of increasing K in the extracellular fluid.
- Hyperosmolarity: Hyperosmolarity causes movement of fluid from inside of the cell to outside. This has a “solvent drag effect”. The fluid moving out carries with it potassium ions causing hyperkalemia.
- Drugs: Certain drugs cause hyperkalemia which includes:
- Potassium-sparing diuretics
- NSAIDs
- Angiotensin-converting enzyme inhibitors
- Angiotensin receptor blockers
- Trimethoprim-sulfamethoxazole
- Heparin
- Impaired Renal Function: This is the most common cause of hyperkalemia. If renal function is mildly deranged, compensatory mechanisms prevent hyperkalemia. But once the glomerular filtration rate falls below 15-20 ml/min there is a significant risk of hyperkalemia.
- Renal tubular acidosis: A condition in which the kidneys are unable to properly acidify the urine associated with hyperkalemia.
- Diabetes Mellitus: Diabetes mellitus is not a cause of hyperkalemia as of itself but leads to conditions that cause hyperkalemia:
- Diabetic diet: Usually high in potassium
- Diabetic Nephropathy: Renal impairment causing hyperkalemia
- ACE inhibitors and ARB can cause hyperkalemia
- Insulin deficiency/insulin resistance: Insulin causes an intracellular shift of potassium reducing plasma potassium. Insulin deficiency, therefore, causes hyperkalemia
- Genetic Diseases:
- Glomerulopathy with fibronectin deposits (GFND)
- Disorders of steroid metabolism and mineralocorticoid receptors
- Congenital hypoaldosteronism
- Pseudohypoaldosteronism
- Disorders of chloride homeostasis
- Nephronophthisis
- Hyperkalemic periodic paralysis (HYPP)
What are the symptoms & signs of hyperkalemia:
Most patients with hyperkalemia are asymptomatic. Patients may complain of non-specific symptoms like weakness, fatigue, nausea, and vomiting.
Rarely patients may develop palpitations, chest pain, muscle paralysis and shortness of breath. But the reason hyperkalemia needs the be taken seriously and treated promptly is that it causes cardiac arrhythmias which can occur without warning and at any level of hyperkalemia.
How to investigate Hyperkalemia?
- Complete medical History: Especially focus on drug history and the risk factors for renal failure.
- Renal function tests: These include Urea, creatinine, and glomerular filtration rate
- Complete Blood count: Look for thrombocytosis and leukocytosis
- Urine Potassium and osmolality: Check for efficiency of renal excretion of potassium.
- Arterial Blood gases: To check for acidosis that can cause hyperkalemia
- Electrocardiogram: ECG changes vary according to the severity of hyperkalemia.
ECG changes in hyperkalemia:
Hyperkalemia is associated with variable ECG changes. The most common ECG change is “Tall & Tented T-waves” with a short QT interval.

This is followed by a “Prolonged PR interval“, “Increased QRS duration“, and the “P waves disappear”
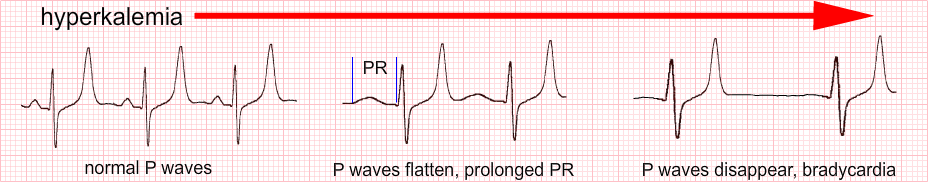
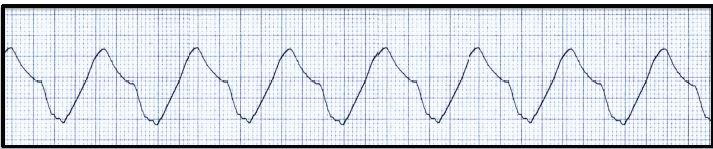
Lastly, the QRS complexes widen and a “sine wave” formation is seen before arrhythmias develop.

Hyperkalemia Treatment:
Hyperkalemia treatment has three important principles.
- Stabilizing the patient
- Removing the excess potassium from the body, and
- Finding and treating the cause
Stabilizing the patient requires cardiac membrane stabilization and rapid shift of the potassium into the cells.
Cardiac membrane stabilization to prevent cardiac arrhythmias:
- Intravenous calcium raises the action potential threshold and prevents arrhythmias.
- 10 ml of 10% Calcium gluconate intravenously over 2-3 minutes is given with continuous cardiac monitoring as calcium gluconate can cause bradycardia, arrhythmias or even cardiac arrest.
- In severe cases, calcium can be given repeatedly until the QRS complexes are normalized.
The intracellular shift of potassium:
- Insulin causes an intracellular shift of potassium from the blood. 10 units of regular insulin are given in 500ml of 10%dextrose water over 60 min in patients with normal blood sugar levels, while in patients with a blood sugar of more than 200mg/dl, 10 units of regular insulin without dextrose water infusion is given.
Blood sugar should be monitored because of the risk of hypoglycemia with this method. Dextrose alone should not be given because of the variable production and release of endogenous insulin.
- Sodium Bicarbonate also has an effect of moving potassium intracellularly and is used to treat hyperkalemia especially in cases with concomitant metabolic acidosis.
- Beta-adrenergic agonists:
Their use is controversial as they produce a lot of side effects however it is an effective treatment for hyperkalemia. The commonly used regimen is Nebulized Albuterol. Side effects include nausea, headache, dizziness, and an increase in blood pressure.
Removal of Excess potassium:
- In patients with a normal renal function, we can give intravenous saline plus a loop diuretic such as furosemide.
- Flurohydrocortisone is a steroid effective against conditions causing hypoaldosteronism.
- Cation exchange resins such as sodium polystyrene sulfonate and Patiromer are novel drugs and cause the elimination of potassium through fecal route.
- Finally, Hyperkalemia which is resistant to all sorts of conservative treatment modalities will require dialysis for correction.
- Lastly, Find the cause of hyperkalemia and treat it accordingly.
- A list of causes has been mentioned above. Treatable causes should be managed. Patients may need dialysis and kidney transplant if the cause is End-stage renal disease.