This presentation about the important causes and symptoms of hypercalcemia has been prepared by our post-graduate resident Dr. Tayyaba Noor.
Approach to Hypercalcemia – Introduction:
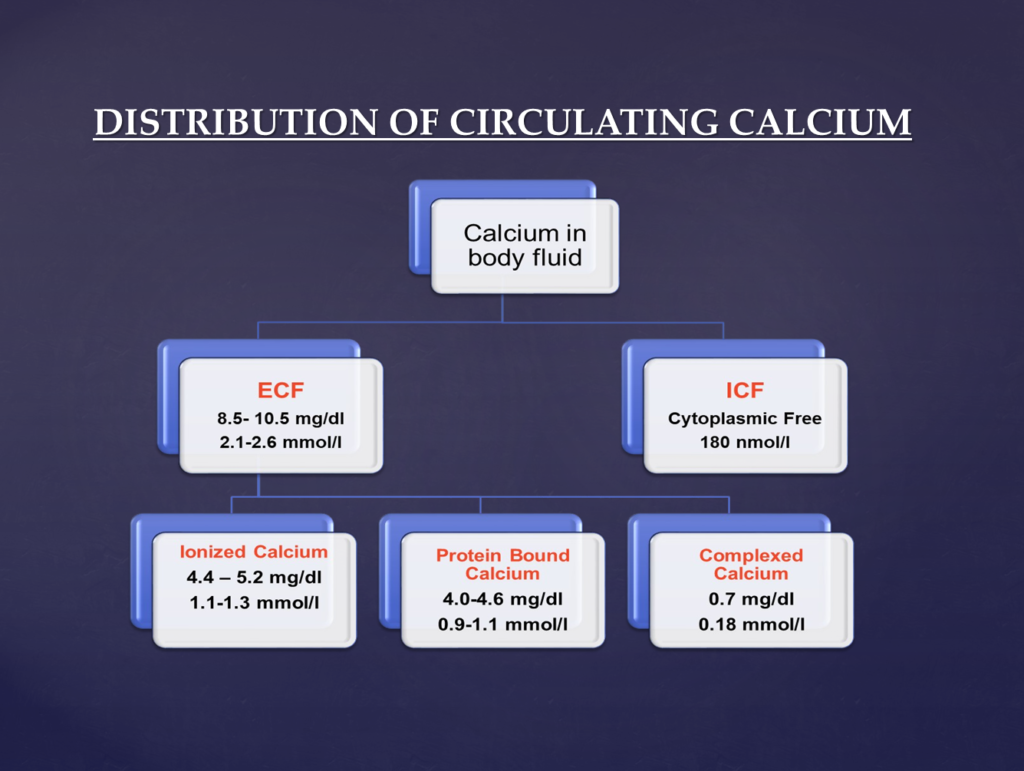
Calcium is one of the most abundant minerals in the human body and it has many important biological functions. 1000-2000 g of Calcium is present normally in the human body out of which 99% is present in the skeleton while the remaining amount is distributed in the ECF and other soft tissues.
The influx and efflux of calcium across the skeletal system occur daily and are mediated by coupled osteoblastic and osteoclastic activity.
Factors Influencing Calcium Levels in the Body:
Calcium in the body is bound to proteins that is primarily influenced by blood pH. Metabolic acidosis decreases the protein binding and increases the ionized calcium in the blood.
On the other hand, metabolic alkalosis increases protein binding of calcium resulting in a reduction in the ionized calcium. Likewise, respiratory alkalosis also decreases the ionized calcium by increasing the affinity of the calcium to bind to proteins.
This effect can be seen in patients with anxiety and panic attacks who hyperventilate during the episode that results in paraesthesias of the hands and perioral numbness. It also can cause carpopedal spasm in severe cases.
It is important to note that the serum calcium increases by 0.1 mmol/L by a 0.1 fall in the blood PH.
Ionized calcium is the active form of calcium and the levels need to be adjusted when the serum albumin and proteins are abnormal such as in patients with malnutrition and malabsorption.
Calcium correction formula:
For every 1 g/dL drop in serum albumin below 4 g/dL, measured serum calcium decreases by 0.8 mg/dL.
Corrected calcium = Measured Calcium in mg/dl + [0.8 x (4 – measured albumin in gm/dl)].
What are the major functions of Calcium in humans?
It causes muscle contraction and is required for neuronal and neuromuscular conduction. It is required for intracellular signaling, bone formation, and bone strength, and as a cofactor for blood clotting (coagulation).
It is also required for enzymatic regulation and maintenance of plasma membrane stability.
How is Calcium Metabolized in the body?
The usual dietary intake of Calcium is 400-1500 mg/day in adults. About 200 to 400 mg of calcium is absorbed from the intestines per day.
The excretion of calcium is regulated by the kidneys and is dependent on the ionized calcium in the blood. Approx 8 to 10 gms of calcium is filtered by the glomeruli daily, out of which only 2 to 3% appears in urine that is equivalent to 200 mg.
65% of the calcium is absorbed in the proximal convoluted tubules while 20% is absorbed in the loop of henle, 10% in the distal convoluted tubules, and 5% in the collecting ducts.

What is Hypercalcemia:
Hypercalcemia is defined as a total serum calcium exceeding 10.5 mg/dl (2.5 mmol/L) or ionized serum calcium exceeding 5.6 mg/dl ( or > 1.4 mmol/L)
Severe hypercalemia is defined as total serum calcium exceeding 14 mg/dl (> 3.5 mmol/L)
Hypercalcemic crisis is the development of severe neurological symptoms or cardiac arrhythmias in a patient with a serum calcium exceeding 14 mg/dl (> 3.5 mmol/L).
The 7 Important Symptoms of Hypercalcemia:
Hypercalcemia or high calcium levels in the blood is usually diagnosed when the patient is being tested for diseases or complications arising from high calcium levels. These may include:
Renal “stones” or Nephrolithiasis:
- These patients may develop severe colicky abdominal pain arising from the flanks or traveling from loin to groin. It may be accompanied by fever and lower urinary tract symptoms such as burning and discomfort while urinating. Some patients may develop diffuse calcifications of the kidneys that is called nephrocalcinosis.
Nephrogenic diabetes insipidus:
- Patients present with excessive urination and thirst. These patients have an increased frequency as well as an increased volume of urination. To make up for the lost fluid via urine, patients tend to drink a lot of water as they get thirsty frequently.
Dehydration:
- Since patients have polyuria or excessive urination, they have an excessive urge to drink water. However, if the patient develops altered mentation or has associated symptoms of vomiting, the patient may become dehydrated.
Skeletal symptoms of hypercalcemia “bones”:
- “Bone pains” is a common symptom. Patients may complain of diffuse skeletal pains and develop fractures because of fragile bones or osteoporosis. Some patients may develop joint pains and swelling.
- Patients may develop a condition called “Osteitis fibrosa cystica”. These patients have subperiosteal resorption and bone cysts when the bony tissue is examined via microscope.
Gastrointestinal symptoms of hypercalcemia “abdominal moans”
- Patients may complain of nausea, vomiting, anorexia, weight loss, constipation, abdominal pain, or develop Pancreatitis.
- The risk of peptic ulcer is greatly increased in the background of hypercalcemia.
Neuromuscular symptoms of hypercalcemia “psychic groans”
- Patients may develop neurological side effects such as impaired concentration, memory impairment, confusion, stupor, and coma. Patients with mild hypercalcemia may only develop lethargy and fatigue.
- Others with long-term hypercalcemia may develop muscle weakness.
Cardiovascular symptoms of hypercalcemia:
- Patients may develop hypertension, ECG changes such as shortened QT interval, and cardiac arrhythmias.
- Vascular calcification can occur as well.
Other symptoms of hypercalcemia:
- Corneal calcification (band keratopathy) may occur secondary to chronic hypercalcemia. patients may also develop keratitis or conjunctivitis.
- Itching is one of the uncommon symptoms of hypercalcemia.
Causes of Hypercalcemia:
Parathyroid hormone-related:
- Primary hyperparathyroidism Sporadic, familial, or associated with multiple endocrine neoplasias I or II
- Tertiary hyperparathyroidism associated with chronic renal failure or vitamin D deficiency
Malignancy
- Humoral hypercalcemia of malignancy (mediated by PTHrP) Solid tumors, especially lung, head, and neck squamous cancers, and renal cell tumors
- Local osteolysis (mediated by cytokines) multiple myeloma, and breast cancer.
Vitamin D-related
- Vitamin D intoxication
- Granulomatous disease sarcoidosis, berylliosis, and tuberculosis
- Hodgkin’s lymphoma
Medications
- Thiazide diuretics (usually mild)
- Lithium
- Milk-alkali syndrome (from calcium antacids)
- Vitamin A intoxication (including analogs used to treat acne)
Other endocrine disorders
- Hyperthyroidism
- Adrenal insufficiency
- Acromegaly
- Pheochromocytoma
Genetic disorders
- Familial hypocalciuric hypercalcemia: mutated calcium-sensing receptor
Other
- Immobilization, with high bone turnovers such as patients with Paget’s disease and bedridden child
- The recovery phase of rhabdomyolysis.
Among all the above-mentioned causes of hypercalcemia, primary hyperparathyroidism and malignancy are the most common, accounting for greater than 90 percent of cases.
Therefore, the diagnostic approach to hypercalcemia typically involves distinguishing between the two.
Patients with hypercalcemia of malignancy usually have higher calcium concentrations and are more symptomatic from hypercalcemia than individuals with primary hyperparathyroidism.
Serum calcium must be corrected for serum albumin before labeling it as a case of Hypercalcemia.