“Bariatric surgery isn’t going to make you lose weight; its a tool to help you lose weight. Half of it is the surgery, and half of it is you eating what you are supposed to eat and exercise.” Ashley Nell Tipton
What is Obesity
Overweight and obesity are defined as abnormal or excessive fat accumulation in the body that presents a risk to health. A crude population measure of obesity is the body mass index (BMI), a person’s weight (in kilograms) divided by the square of his or her height (in meters).
A person with a BMI equal to or more than 25 is considered overweight. A person with a BMI of 30 or more is generally considered obese. Obesity is frequently subdivided into the following categories:
Class 1: BMI of 30 to < 35
Class 2: BMI of 35 to < 40
Class 3: BMI of 40 or higher.
Class 3 obesity is sometimes termed as “morbid” “extreme” or “severe” obesity.
BMI of over 50 is usually considered super obese.
Asian populations develop negative health consequences at a lower BMI than Caucasians, consequently some nations have redefined obesity. The Japanese have defined obesity as any BMI greater than 25 while China uses a BMI of greater than 28.

Diseases linked to Obesity
People who are obese, compared to those with a normal or healthy weight, are at increased risk of developing many serious diseases and health conditions.
It is estimated that a severely obese male at age 21 will live 12 years less and a woman 9 years less than a non-obese individual. Some of the common disease directly linked to obesity are:
- High blood pressure (Hypertension)
- High LDL cholesterol, low HDL cholesterol, or high levels of triglycerides (Dyslipidemia)
- Type 2 diabetes
- Coronary heart disease (Heart Attack)
- Stroke
- Gallstones
- Osteoarthritis (a breakdown of cartilage and bone within a joint)
- Sleep apnea and breathing problems
- Heart burn and hiatal hernia.
- Some cancers (endometrial, breast, colon, kidney, gallbladder, oesophageal and liver)
- Infertility
- Excessive body hair growth, polycystic ovaries, and irregular menstruation in females
- Urinary stress incontinence
- Low quality of life
- Mental illness such as clinical depression, anxiety, and other mental disorders
- Body pain and difficulty with physical functioning.

How to fight against Obesity:
The treatment of obesity begins with lifestyle modification. This includes changing the bad eating habits to take a balanced, healthy diet rich in vegetables, salads, and fruits. Refined carbohydrates, sugars, carbonated drinks, sweets, and deep fried food are few sources of unhealthy high caloric intake that result in excessive weight gain.
Another important factor to reduce weight is to increase physical activity and regular exercise to burn an extra amount of fat accumulated in the body.
Unfortunately, the long-term success rate for the severely obese people that tries dieting and exercise as a mean of losing enough weight to no longer be obese and maintaining that weight loss is only approximately 3%.

Bariatric surgery
Bariatric surgery is offered to patients who have BMI of 35 and above, or lower BMI of 30 and a comorbid condition like diabetes or hypertension, with at least two documented attempts of weight loss failure by lifestyle and dietary modification.
In bariatric surgery, certain changes are made to the stomach or small intestine, or both. Research has shown weight loss that follows after bariatric surgery leads to remission of type 2 diabetes, high blood pressure, dyslipidemia and many more obesity-related diseases. Here are few of commonly offered bariatric surgical procedures.

Laparoscopic Sleeve Gastrectomy (LSG)
Gastric sleeve surgery is one of the relatively newest procedures and is fast gaining in popularity. The surgery makes the stomach smaller so individuals feel full faster. In this surgery more than half of the stomach is removed, leaving a narrow vertical sleeve, or tube of approximately 150 ml capacity.
Surgical staples keep the new stomach closed. Because part of the stomach has been removed, this procedure is not reversible.
After surgery, the patient will need to make lifelong changes in eating habits that include eating smaller portions. However, that shouldn’t be a challenge because research shows that this surgery causes favorable changes in gut hormones that suppress hunger, reduce appetite and improve satiety.
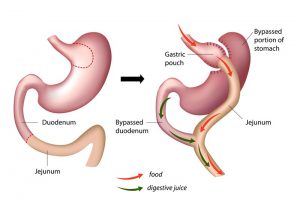
Roux-en-Y Gastric Bypass Procedure (RYGB)
This procedure uses a combination of restriction and malabsorption. A small stomach pouch is created and attached to a Y-shape fashioned section of the small intestine as shown in the diagram. This permits food to bypass a large portion of the small intestine, which absorbs calories and nutrients.
The smaller stomach pouch makes patients feel fuller sooner and eat less food; the patient absorbs fewer calories because the food bypasses a portion of the small intestine leading to weight loss.
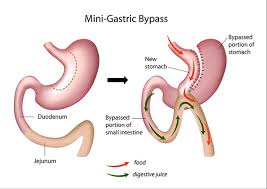
Mini gastric Bypass (MGB)
The mini gastric bypass procedure was first developed by Robert Rutledge from the US in 1997, as a modification of the standard Billroth II procedure. A mini gastric bypass creates a long narrow tube of the stomach along its right border (the lesser curvature).
A loop of the small gut is then brought up and joined to this tube usually at about 150 cm to 200 cm from the start of the intestine.
The MGB has been suggested as an alternative to the Roux en-Y procedure due to the simplicity of its construction and is becoming more and more popular because of low risk of complications and good sustained weight loss.
It has been estimated that about 15% of weight loss surgery in Asia is now performed via the MGB technique.
Read More …
How to lose weight fast without pills
Weight gain may be a symptom of an underlying disease
Lumbar puncture procedure – Technique, Indications, and contraindications