This is another interesting case of 32 years of age female, a diagnosed case of cardiomyopathy, who was admitted in our ward with a petechial skin rash which developed after she was prescribed rivaroxaban by a cardiologist for atrial fibrillation.
History of the patient …
The patient was labeled as a case of cardiomyopathy for the past two years and she was on the typical cardiologist’s cocktail treatment for that.
She had leg swelling, shortness of breath, orthopnea, and PND but these symptoms were relieved with diuretics and other treatment prescribed by the cardiologist.
Cardiomyopathy with Atrial fibrillation
One month back she developed palpitations and went to her cardiologist again. Her ECG and echocardiography were performed and she was found to have atrial fibrillation for which she was started on rivaroxaban 15 mg twice daily apart from her usual medications for cardiomyopathy.
After initiation of rivaroxaban, she developed petechiae, purpura, and bleeding from gums. She was brought to PIMS emergency and was admitted in our ward.
Apart from the bleeding tendencies and shortness of breath, the patient did not have any systemic complaints like fever, skeletal pains, abdominal symptoms, jaundice, and arthralgias, etc.
The patient was recently labeled as a case of type 2 Diabetes Mellitus and was on oral antidiabetic medicines with good control. She also had amenorrhea for the past few months.
Diabetes & Splenomegaly
Two years back, she was investigated for some abdominal symptoms and was told that she had splenomegaly. However, she denied any symptoms associated with it.
On Examination …
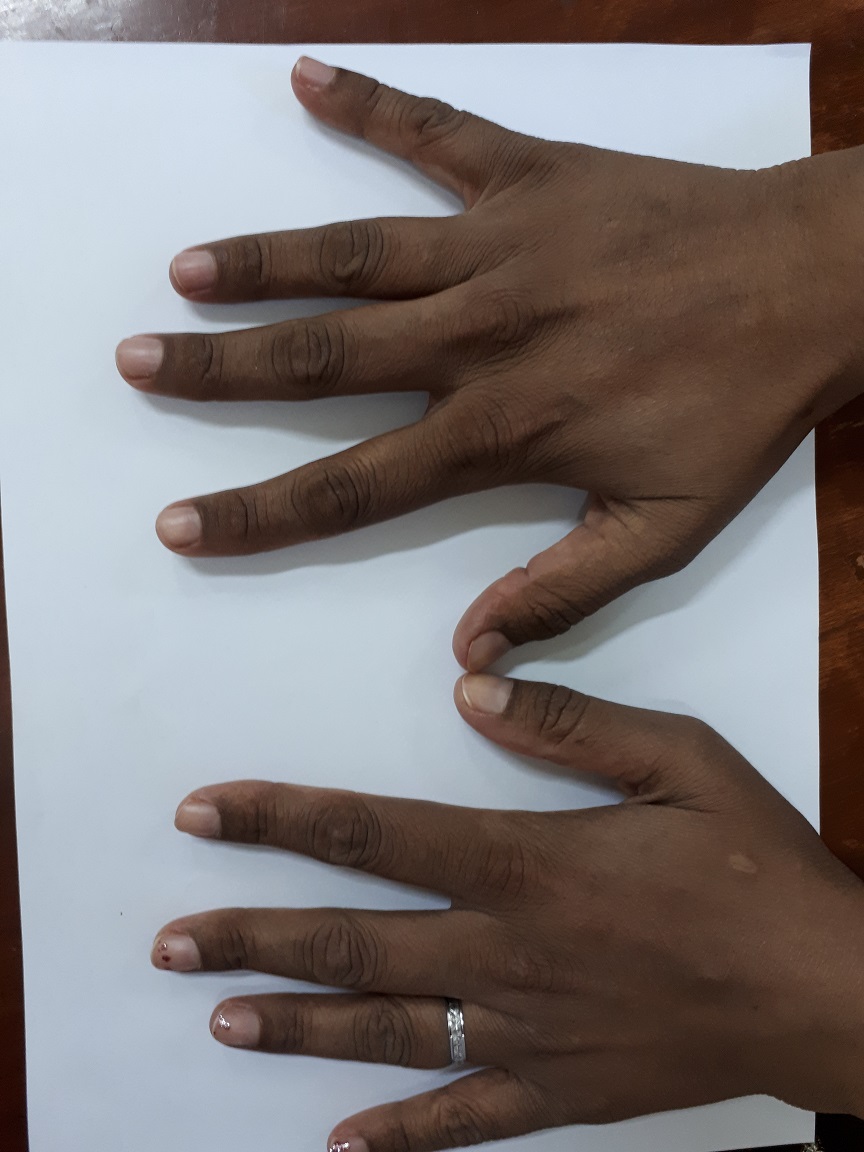
On examination, she was dyspneic and could not lie down. She had petechiae and purpura over the lower limbs and had generalized body pigmentation.

She had an irregular pulse and bibasal crepitations with raised Jugular venous pulsations.
Abdominal examination revealed a firm splenomegaly of 6 cm without any evidence of free fluid in the abdomen. Systemic examination was otherwise unremarkable.
The patient was resuscitated and treated for heart failure with intravenous diuretics, oxygen, and digoxin. She was transfused with platelets and tranexamic acid was given.
Investigations of the patient …
The patient ECG showed fast atrial fibrillation. Other investigations are as follows:
- Blood CP:
- Hemoglobin: 10.5 gm/dl
- MCV: 97 fl
- Reticulocytes: 3%
- WBCs: 6200/ul
- Platelets: 0/ul
- Chemistry:
- Blood sugars: 97 mg/dl
- Glycated hemoglobin: 5.4%
- Bilirubin: 0.6 mg/dl
- ALT: 132 U/l
- Alkaline phosphatase: 140 U/l
- Urea: 40 mg/dl
- Creatinine: 1.2 mg/dl
- Uric Acid: 7.2 mg//dl
- Chest X-ray:
- Cardiomegaly
- Ultrasound abdomen:
- Hepatic steatosis
- splenomegaly
- mild ascites
- Normal portal veins
- Bone marrow Biopsy:
- Excessive peripheral destruction
- Echocardiography:
- Mild MR, AR, TR
- Ejection Fraction: 50%
What further investigations should be performed in this patient?
What is the likely diagnosis?
How should she be managed?
The answer will be posted after a few days …
Keep guessing. write your comments below?
Date: 26/05/2019
Let’s proceed the case further …
Since the patient was in heart failure, initial treatment aimed at improving her dyspnea. She was started on intravenous diuretics, Oxygen, Digoxin, and nitrates.
She was transfused with platelets as her platelets count was “ZERO” and she was actively bleeding.
She was started on short-acting insulin for diabetes along with other supportive treatments.
Further labs were advised to look for the underlying cause after she was stable.
Serum Iron: 303 ug/dl (Normal: 50 – 170)
Serum TIBC: 43 ug/dl (Normal: 250 – 450)
Trasferrin saturation: 704 % (Normal: 12 – 45%)
Serum Ferritin: 1500 ng/ml (10 – 120)
LH & FSH were Normal while estradiol levels were very low.
Cardiac MR was advised, however, it was not performed because of non-availability and non-affordability.
HFE gene mutations were sent to another hospital but again that was too costly and could not be performed.
Liver Biopsy was planned once the platelets improve.
She was labeled as a case of:
Hemochromatosis with dilated cardiomyopathy, secondary (Bronze) Diabetes, Liver Cirrhosis (Child Class B), and Hypogonadotropic Hypogonadism.
The patient was started on oral iron chelation in the form of Asunra (Deferasirox 400 mg twice daily) along with spironolactone, low dose Beta-Blocker, and other supportive treatment.
We planned to give her GnRH (gonadotropins) for central hypogonadism after a few months if she does not improve with iron chelation alone.
A brief discussion about hemochromatosis and indications for anticoagulation in patients with atrial fibrillation will follow soon.
Where are the treatment lapses in the management of this patient?
Can we add anything to the treatment regimen that will help our patient?
Your input will be highly appreciated …
Read More …
The new definition of myocardial infarction