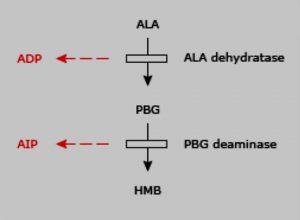
Acute Intermittent Porphyria is an autosomal dominant disorder resulting from a partial deficiency of PBG (porphobilinogen deaminase).
Acute intermittent porphyria affects the central nervous system, peripheral, somatic and autonomic nervous system. Patients may present with intermittent attacks which may be life-threatening at times.
Clinical features of Acute intermittent porphyria:
Acute intermittent porphyria as the name suggests is characterized by intermittent attacks of symptoms with rapid onset of symptoms, hence the term “acute”. Symptoms may be visceral, autonomic, psychiatric or neurological and peripheral.
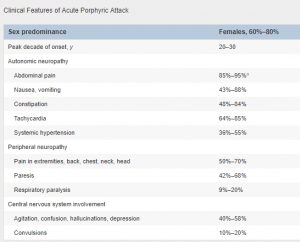
Abdominal pain is the most common symptom. It is usually severe but tenderness, fever, and leukocytosis are minimal.
The pain may mimic acute appendicitis, mesenteric ischemia, and as the acute surgical abdomen. In fact, surgical exploration is the fate of many patients who present with abdominal pain.
Other symptoms include numbness, paraesthesias, and neuropathy.
Motor weakness usually starts in the proximal muscles and progress to distal muscles.
Patients may present with bladder dysfunction, constipation or diarrhea. The Urine changes its color to black or reddish-brown on exposure to sunlight. Other patients may develop hallucinations, agitation, and depression.
Some patients may develop hyponatremia and hypomagnesemia. Hyponatremia is usually due to the syndrome of inappropriate anti-diuretic hormone. Patients may also have fluctuating blood pressure or may develop hypertension.
In patients with bulbar and respiratory muscles involvement, AIP may be life-threatening.
Diagnosis of Acute intermittent porphyria:
Urine for PBG is the most cost-effective test to diagnose AIP. PBGD deficiency may be identified via DNA testing after the diagnosis of AIP.
Treatment of AIP:
Hospitalization is usually required for acute attacks.
Patients should be monitored for respiratory failure. Electrolytes and nutritional status should be assessed and managed accordingly.
Tachycardia and hypertension may be treated with propranolol. Pain and nausea may require narcotic analgesics and ondansetron.
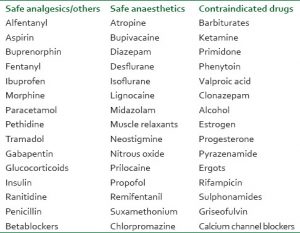
Almost all anti-epileptics are known to exacerbate the condition. Hyponatremia may require hypertonic saline and free water restriction. Similarly, patient with seizures and hyponatremia should be managed with hypertonic saline first. If the seizures are still not controlled after the correction of hyponatremia, clonazepam may be used as an anti-epileptic.
Attacks should be treated with carbohydrates and hemin.
Liver transplantation is very effective but there have been reports of worsening neurological symptoms after liver transplantation.
The patient should be advised to take a high carbohydrate diet, avoid oral contraceptive pills and most of the neuropsychiatric medicines.