Vaginal yeast infection is a common problem in women and is second only to bacterial vaginosis as a cause of vaginitis. It is also called yeast vaginitis or vaginal candidiasis.
Unlike Trichomonas
Vaginal yeast infection – How do we acquire it?
Candida species ( the most common yeast responsible for candida vaginitis) is present in up to 20% of normal healthy asymptomatic females. It is most common in the reproductive age group i.e. menstruating women.
They are less common in the postmenopausal and prepubertal females. It is thought that candida probably accesses the vagina from the perineal area and rectum. Less common causes include recurrence of a vaginal reservoir and sexual transmission.
What are the symptoms of vaginal yeast infection?
Patients may present with any one or more of the following vaginal symptoms:
- Itching around the vaginal opening and irritation of the vulva is the main symptom.
- Vulval soreness and pain may accompany itching in severe cases
- Dysuria or painful urination
- Painful sexual intercourse
- Abnormal thick whitish (curd-like) discharge without bad odor. Vaginal discharge may be absent in some patients.
How to differentiate between vaginal yeast infection and other vaginal infections?
Symptoms of
| Characteristics | Possible causes |
| Scanty thin, watery white discharge | Atrophic vaginitis |
| Thin, green or gray-white, foul-smelling discharge | Bacterial vaginosis |
| Profuse white curd-like discharge with yeasty odor | Candidiasis |
| Mucopurulent, foul-smelling d | Chancroid |
| Yellow, mucopurulent, odorless or acrid discharge | Chlamydial infection |
| Scant serosanguineous or purulent discharge with foul odor | Endometritis |
| Copious mucoid discharge | Genital herpes |
| Profuse mucopurulent discharge, possibly foul smelling | Genital warts |
| Yellow or green, foul-smelling discharge | Gonorrhea |
| Chronic, watery, bloody or purulent discharge (maybe foul smelling) | Gynecologic cancer |
| Frothy, green-yellow, and profuse foul-smelling discharge | Trichomoniasis |
Which patients are at risk of developing a vaginal yeast infection?
Most women with the disease are healthy and have no comorbid disease. However, yeast infections may be more common in a subgroup of patients who have the following risk factors:
- Diabetes: Diabetic patients have a high incidence of bacterial and fungal infections. A number of patients are found to have diabetes when they develop vaginal yeast infection or oral thrush. https://www.fever.pk/complications-diabetes-mellitus/
- Long-term use of antibiotics: the use of antibiotics, especially on a long-term basis, lead to clearance of the bacteria that normally reside in the vagina. Loss of the normal vaginal flora leads to overgrowth of yeast.
- Patients using birth control pills: Estrogen-containing birth control pills are especially associated with the growth of vaginal yeast infection.
- Patients using contraceptive devices: intrauterine devices are associated with an increased risk of vaginal yeast infections. There is no association of yeast overgrowth in patients using spermicides although vaginal irritation is commonly seen.
- Those on immunosuppressants/ or have a weak immune system: A good immunity prevents a person from opportunistic infections. Patients who are immunocompromised as those using steroids, HIV positive and other immunosuppressants are highly likely to develop yeast infections among other bacterial and viral infections.
- Pregnancy: vaginal discharge may be more common in pregnant patients. This may or may not be secondary to a yeast infection.
- Sexually active patients: Vaginal yeast infection is commonly seen in patients who are sexually active. It is not a sexually transmitted disease but sexually active women have hormonal changes in their bodies that make them prone to develop yeast infections.
All the above risk factors when present, makes the female prone to develop a
How to diagnose vaginal candidiasis?
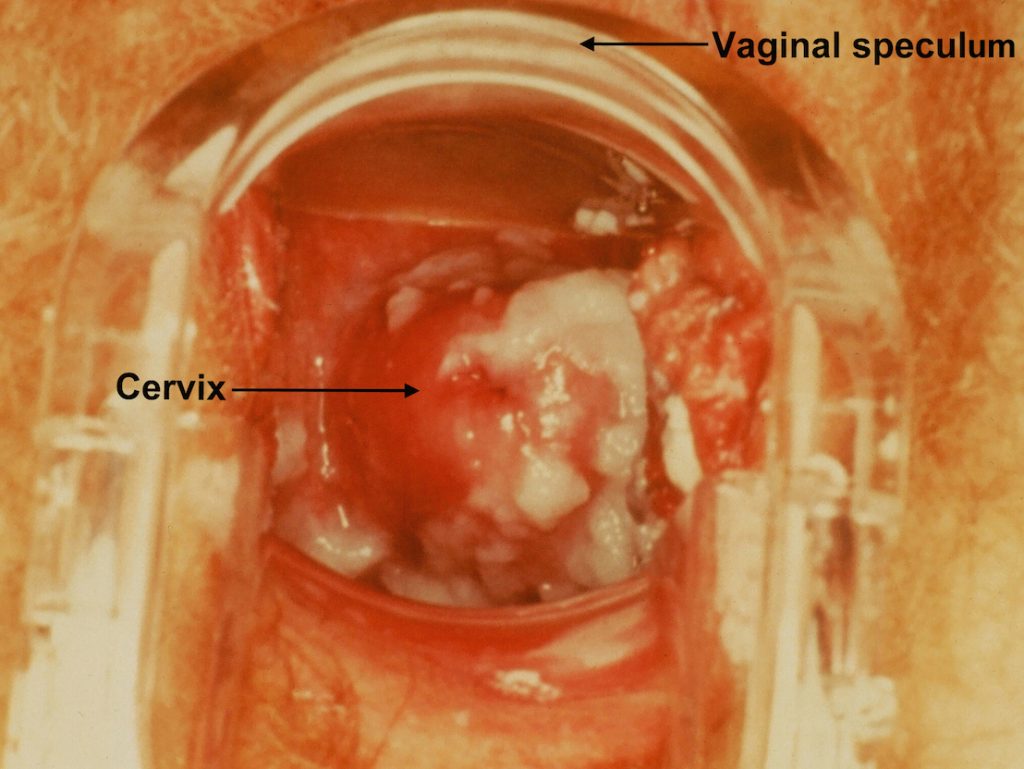
Yeast infections can be diagnosed by your doctor after examining the vagina and taking a sample for microscopic examination. Self diagnosis is usually not correct and should be discouraged.
How to treat the vaginal yeast infection?
A variety of topicl and oral antifungal treatments are available over the counter. Topical treatment relieve symptoms rapidly and are not associated with gastrointestinal and systemic side effects. However, oral treatment can be used as a single pill and is thus easy to take. Furthermore, women find it more convenient to take a pill than vaginal application.
Patients who have a complicated vaginal yeast infection should take the medicines for a longer duration. The following group of patients may require a prolonged antifungal therapy:
- Severe vaginitis: oral fluconazole 150 mg every third day (total 3 doses) or topical antifungal for 7 days.
- Recurrent vaginal candidiasis: oral fluconazole every third day (3 doses), followed by weekly for 6 months or topical azoles for 14 days then twice weekly for 6 months
- Compromised host (poorly controlled diabetes, immunosuppression,
and debilitated patients): oral or topical therapy for 14 days - Pregnancy: intravaginal clotrimazole or miconazole for 7 days
Yeast infection while pregnant:
Vaginal yeast infection is not associated with worse pregnancy outcomes. Patients should be treated with intravaginal miconazole or clotrimazole for 7 days.
Oral azoles are contraindicated during the first trimester because of
Probiotics and boric acid have not been proven to be effective. Treatment of the male partner is not necessary.
Breastfeeding women should ideally be given nystatin. Fluconazole enters the breast milk but has not been found to cause any adverse effects in neonates. Fluconazole can be given during breastfeeding. Topical application of azoles can be safely used as absorption is minimal, however, oral azoles should be avoided.
How does vaginal candidiasis affect the male partner?
Post-coital hypersensitivity reactions may occur in the male partner. This is manifested by redness, itching, and inflammation of the penis. Male partners do not require treatment. Topical application of low potency steroids may relieve the symptoms.
Treatment of the sexual partner is not necessary and there is no contraindication to sexual intercourse during the treatment but may be uncomfortable because of the soreness and inflammation.
To summarize …
Vaginal yeast infection is common healthy females. Women who have diabetes, are immunocompromised, are sexually active and use contraceptive pills or devices are especially at risk of developing recurrent infections. Symptoms include vaginal discharge, itching, painful micturition and sexual intercourse. Treatment includes topical azoles and oral fluconazole as a single tablet in uncomplicated cases.