Behçet’s disease is also called as the “silk route” disease. The name Behcet’s disease is named after the Turkish dermatologist Hulusi Behçet who published the characteristic findings of Behcet’s disease in 1937. It is also called as the “Silk route” disease because of the prevalence of this disease in the areas surrounding the ancient silk routes in the middle east and central Asia. It is most common in Turkey where its prevalence ranges from 80 to 370 cases per 100000 population.
Clinical features of Behcet’s disease
Most clinical manifestations are believed to be due to vasculitis but thrombosis due to a hypercoagulable state is not uncommon. Vasculitis in Behcet’s disease involves blood vessels (both arteries and veins) of all sizes.
The disease typically affects young adults of both genders. Sporadic cases are common but familial clustering and genetic anticipation has been described. Severity is generally greater in males. Compared to other vasculitides, renal and peripheral nervous system vasculitis is a rare finding in Behcet’s disease.
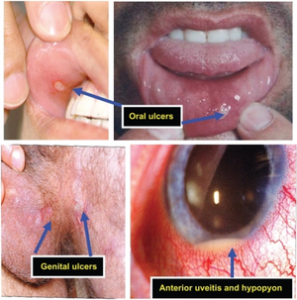
Oral ulcerations in Behcet’s disease
Majority of patients present with recurrent oral aphthous ulcers (canker sores). The clinical and histological appearance of these oral ulcers is similar to the benign oral ulcers but these tend to be multiple and extensive. Ulcers in Behcet’s disease are painful and may leave a scar. These ulcers are recurrent and occur more than three times a year and heal within two to three weeks.

Genital ulcers in Behcet’s disease
Like oral ulcers, genital ulcers are frequent manifestations of the disease. These ulcers are similar in appearance to the oral aphthae and are usually painful. Scrotum in males and vulva in women are frequently involved in this disease.
Cutaneous lesions in Behcet’s disease
Skin manifestations vary and may include acneiform lesions, papulo-vesiculopustular eruptions, pseudofolliculitis, nodules, erythema nodosum (septal panniculitis), superficial thrombophlebitis, pyoderma gangrenosum-type lesions, erythema multiforme-like lesions, and palpable purpura.
The Pathergy test:
Pathergy refers to an erythematous papular or pustular response to local skin injury. It is defined as a pustule-like lesion or papule that appears 48 hours after skin prick by a 20 gauge needle.


Ocular disease in Behcet’s disease can lead to blindness

Ocular presentations (anterior or posterior uveitis, hypopyon, retinal vasculitis, cystoid macular degeneration) represent the first manifestation of disease in 10% of patients with Behçet disease but usually occur following oral ulceration. Uveitis is the dominant feature, highly recurrent and can lead to blindness. Other changes include conjunctivitis, scleritis, episcleritis, sicca syndrome, glaucoma, secondary cataracts, conjunctival ulceration, and neovascularization. Retinal vasculitis may be severe and vision-threatening and may require treatment with immunosuppression
Neurologic disease in Behcet’s disease
Neurological involvement is more common in men. Apart from focal neurologic lesions and thrombosis, patients may present with seizures, aseptic meningitis, encephalitis arterial vasculitis, personality change, and dementia may develop. Arteritis may lead to ischemic strokes, dissection, and subarachnoid hemorrhage. Unlike other vasculitides, peripheral neuropathy is less common in Behcet’s disease
Vascular disease in Behcet’s disease
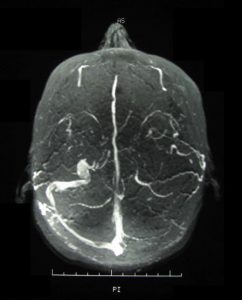
Vascular disease in Behcet’s disease is more common in men. Characteristically it involves both arterial and venous system and vessels of all sizes. However, venous disease is more common than arterial. Patients can present with Budd-Chiari syndrome, inferior and superior vena cava occlusion, dural sinus thrombosis and deep vein thrombosis of the lower limbs. The pulmonary arterial system is particularly a characteristic feature and requires early recognition. Patients may present with a cough, dyspnea, pleuritic chest pain, and hemoptysis. Coronary vasculitis is uncommon however acute myocardial infarction in Behcet’s disease has been reported.
Hughes-Stovin Syndrome
Pulmonary artery thrombosis and aneurysms in association with peripheral thrombophlebitis are known as Hughes-Stovin syndrome, and this syndrome most commonly occurs in Behçet’s disease and may represent a part of the spectrum of manifestations seen in Behçet’s disease.
Arthritis in Behcet’s Disease
About half of the patients may develop arthritis. Arthritis is usually non-erosive, non-deforming and asymmetric and occurs particularly during exacerbations. Arthritis most commonly affects the medium and large joints, including the knee, ankle, and wrist. Like oral ulcerations, arthritis typically lasts one to three weeks.
Renal disease in Behcet’s Disease
Renal involvement in Behçet’s disease is less frequent and often less severe than in other types of vasculitis. Patients with renal disease may have proteinuria, hematuria, or mild renal insufficiency but can progress to renal failure.
Cardiac disease in Behcet’s disease

Cardiac involvement in Behcet’s disease includes pericarditis, myocarditis, coronary arteritis with or without myocardial infarction, coronary artery aneurysms, atrial septal aneurysm, conduction system disturbances, ventricular arrhythmias, endocarditis, endomyocardial fibrosis, mitral valve prolapse, intracardiac thrombosis, and valvular insufficiency. The atherosclerotic disease like in other autoimmune diseases is less common.
Gastrointestinal ulcerations in Behcet’s diseases

Gastrointestinal ulcerations occur in some patients with Behçet’s disease, and intestinal perforation can occur. Discrete ulcerations are most often seen in the terminal ileum, cecum, and ascending colon. Oral ulcers frequently occur in patients with inflammatory bowel disease that are indistinguishable from the oral aphthae of Behçet’s disease; thus, inflammatory bowel disease needs to be considered before making the diagnosis of Behçet’s disease. Other manifestations include anorexia, nausea, vomiting, abdominal pain, and diarrhea.
Pulmonary disease in Behcet’s disease
Pulmonary parenchymal disease includes loss of lung volume, well-defined opacities, and indistinct nodular or reticular shadows. Other findings include pleural effusion, pulmonary arteritis or venulitis, bronchial stenosis, abscess, obstructive airway disease, chronic bronchitis, and fibrosis.
Pregnancy in Behcet’s Disease
Behçet’s disease in pregnancy has not been studied well. Smaller studies report no change in the outcome but the risk of abortion is high.
Diagnosis of Behcet’s disease

Diagnosis is mainly clinical. Inflammatory markers like ESR and CRP may be raised.
The international study group (ISG) criteria, published in 1990 is the most widely used and accepted criteria among experts.
They require the presence of recurrent oral aphthae (at least three times in one year) plus two of the following in the absence of other systemic diseases:
- Recurrent genital aphthae (aphthous ulceration or scarring)
- Eye lesions (including anterior or posterior uveitis, cells in vitreous on slit lamp examination, or retinal vasculitis observed by an ophthalmologist)
- Skin lesions (including erythema nodosum, pseudo-vasculitis, papulopustular lesions, or acneiform nodules consistent with Behçet’s)
- A positive pathergy test
Pathergy is defined by a papule 2 mm or more in size developing 24 to 48 hours after oblique insertion of a 20 gauge needle 5 mm into the skin, generally performed on the forearm.
Crohn’s disease, ulcerative colitis, and familial Mediterranean fever share some clinical manifestations with Behçet’s disease
Treatment and recommendations:

Minor disease manifestations
Minor disease manifestations are those that interfere substantially with patients’ quality of life but do not threaten vital organ function. Examples of minor disease manifestations are arthritis and mucocutaneous disease.
- For arthritis, oral aphthae, genital ulcers, and other skin manifestations that are relatively mild, colchicine may be preferred as the initial therapy ( Grade 2B ). The typical daily dose ranges from 1 to 2 mg.
- Consider glucocorticoids or other immunosuppressive agents early in the course of erythema nodosum and pyoderma gangrenosum (Grade 2C ).
- For minor disease manifestations not responsive to colchicine, systemic glucocorticoids may be required. The dosing of glucocorticoids depends on the specific clinical indication.
Major disease manifestations
Major disease manifestations are those that may lead to the dysfunction of major organs and even to death. These include certain ocular and neurological manifestations, as well as complications of large-vessel arteritis and venous thrombotic disease.
- Anterior uveitis must be treated with topical corticosteroids with a mydriatic (eye dilating) agent to prevent synechiae formation between the iris and lens. Scopolamine (0.25 percent) or cyclopentolate (1 percent) is usually used for this purpose.
- Posterior uveitis poses a major threat to vision. Treatment should be initiated as soon as possible with both high-dose glucocorticoids and a second immunosuppressive agent ( Grade 1B )
- For organ or life-threatening disease, prednisone dose of 1 mg/kg per day, not to exceed 80 mg/day may be initiated. Pulse therapy with intravenous methylprednisolone (1 g/day for three days) may be used empirically for organ- or life-threatening disease.
- Azathioprine, infliximab, cyclophosphamide, and cyclosporine may be used as a second line and as steroid-sparing agents ( Grade 2 C). Other options that may be utilized include interferon alfa and other anti-TNF agents.
- Among the neurological manifestations, encephalitis, medium-vessel vasculitis, and focal parenchymal lesions of significant size should be treated in the same manner as posterior uveitis ( Grade 2C ).
- Arterial involvement in Behçet’s disease sometimes leads to dilatations and aneurysms of medium- and large-sized arteries. These complications may require combined medical and surgical or interventional radiology treatments. Unless intervention is required urgently, it is prudent to postpone invasive approaches to these vascular complications until the inflammatory component of Behçet’s disease has been controlled with medical therapy.
- Venous thrombotic events in Behçet’s disease are believed to be related to vascular inflammation rather than inherent problems with coagulation. Thus, anti-inflammatory approaches to therapy are appropriate simultaneous to anticoagulation.
Read more …
A real case scenario of Behcet’s disease
A very interesting case of secondary hypertension
Vitamins deficiency can cause oral ulcers too